Re: Blood Oxygen
As we all know that we can last max ten minutes without Oxygen and when people are struggling to breathe and desperate for Oxygen, the medical procedure is to give the patient an Oxygen Mask if they can breathe on their own or Intubate the patient shove a big fat tube down the throat gagging the patient and preventing him for eating swallowing or speaking. Nice way to kill a sick person in my Opinion.
Every time a patient dies of covid in a Hospital ICU I believe it is not the covid that killed the patient but the intubation and humongous stress put on lungs already suffering from Pneumonia .
There has to be a better way to maintain blood oxygen levels by bypassing the already stressed lungs
My question is " If Drips are used to add Saline solutions, Blood Plasma, Blood Transfusions, Platelets, we can even take all the blood out and pass it through a machine for Dialysis, we can give antibiotics using drips not to forget Iron In fusion directly into the Blood which I received for the second time today. This being the case WHY CANNOT BLOOD be Oxygenated directly using DRIPS by passing the already struggling lungs.
Imagine Patients suffering from Cystic Fibrosis of the lungs on a respirator ?
Is there a reason why this is not possible ?
This is my new Research Topic.
My search is not to substitute the function of the human lung as it is part of an autonomic system. We breathe automatically 24/7 whether we are awake or asleep or even unconscious. No human being cal live without Oxygen for more than 5 minutes or so. The effort of mine is to find ways and means to add more oxygen to the system boosting a failing lung heart autonomic system, especially say for Covid Patients right now as we speak.Many hospitals I am aware use Sleep apnea machines to assist breathing but may not be the right option as it puts enormous pressure on weakened lungs
If you have any valuable suggestions kindly drop me a note
My Assumption:
Engineers and Technologists are the Brains behind each and every medical gadget that gets used in this century.
Burnstein was an Electrical Engineer born with Type1 diabetes and almost lost his life several times due to Diabetic Hypoglycemia & Keto acidosis and wanted to take charge of his diabetes and stay alive. When the Going gets tough, the Tough get Gpoing, so he decided to study medicine and became an Endocrinologist too as a Mature age student and he battled with FDA to allow Patients to Monitor Blood sugar levels at home using little portable machine with strips. The Medical Profession was dead against it.
For support during high-risk procedures in the cardiac catheterization lab.
As a bridge to a heart assist device, such as left ventricular assist device (LVAD).
As a bridge for patients awaiting lung transplant. The ECMO helps keep tissues well oxygenated, which makes the patient a better candidate for transplant.
Procedure
Being placed on ECMO requires a surgical procedure but it is usually done in a patient's room. The patient is sedated and given pain medication and an anti-coagulant to minimize blood clotting. A surgeon, assisted by an operating room team, inserts the ECMO catheters into either an artery or veins. An x-ray is then taken to ensure the tubes are in the right place. Usually a patient on the ECMO pump will also be on a ventilator, which helps the lungs to heal. While on ECMO, the patient will be monitored by specially trained nurses and respiratory therapists, as well as the surgeon and surgical team. Since you will be sedated and have a breathing tube in place, supplemental nutrition will be provided either intravenously or though a nasal-gastric tube. Nutrition is delivered either intravenously or though a nasal-gastric tube
While on ECMO, you may be given certain medications including: heparin to prevent blood clots; antibiotics to prevent infections; sedatives to minimize movement and improve sleep; diuretics to help the kidney get rid of fluids; electrolytes to maintain the proper balance of salts and sugars; and blood products to replace blood loss.
xxxxxxxxxxxxxxxxx
Dr.Sachitra - Sydney
Uncle sorry dint get time to reply...had me thinking...
Coz in my field i know intubation only has saved so many lives... Yes it has its downfall and disadvantages especially if u don't know how to ventilate, but now a days the understanding is so much better regarding all this.
There is a way where we can oxygenate outside which is called ECMO...its so expensive. Even in countries like ours there are certain indicators when u can put on ecmo
xxxxxxxxxx
Er. Manju Gupta
Regarding your Research Topic on oxygen intubation, yes I wholly agree that such practice can suffocate a patient. Agree that such infusion of oxygen rich blood after having been thru a enrichment process would benefit a patient.
After the patient is dead we cannot carry out a enquiry to ask him if he felt difficulty in breathing once a tube is pushed down his throat.
Technically this plasma or hameoglobin enrichment process is feasible - only such research to invent a machine is necessary , like dialysis .
Good thinking . Manju
xxxxxxxx
Dr.Manjula Krishnaswamy ( My surgeon Sister)
The process of oxygenation is a complex process of the haem molecule exchanging gases which happens in the lung. It is not simple diffusion of oxygen into the blood / plasma. It's only haemoglobin in the blood that carries oxygen or cabondioxide
xxxxxxxxxxxxx
Er. Anand Rangarajan:
This machine is called the heart/lung machine. It’s just too expensive to implement
xxxxxxxxxxxxxx
Amaresh Simhadri :
I don't have a suggestion but it's a good topic for research. On this why do you think none of the scientist didn't think of it,?
xxxxxxxxxxxxxx
xxxxxxxxxxx
Parexel India Symposium
25 November 2021 @ 05:00 PM
Virtual Event





Register Now
ECMO is a vital tool but it requires highly trained staff and a huge amount of hospital resources. Patients who survive ECMO support may have long term health complications related to their critical illness.
Outsourcing the heart and lungs
In lay terms, ECMO is a heart or lung bypass machine. A pump and artificial lung, both sitting outside the body, provide a level of support the sick organs can no longer provide. This way, the rest of the body's functions are maintained.
The meaning of each of the letters of the ECMO acronym is:
Extra Corporeal: outside the body
Membrane: the artificial lung is referred to as a “membrane”, or thin layer of material that keeps blood flowing on one side and oxygen on the other. This thin and porous membrane allows oxygen in and carbon dioxide out
Oxygenation: when oxygen enters the blood it is equivalent to breathing in. The process equivalent to breathing out, the removal of carbon dioxide, also occurs.
As well as the oxygenator, the ECMO machine includes cannulae – or tubing – to drain the blood from the patient and return it once oxygen has been added and carbon dioxide removed, a pump and a control panel.
ECMO evolved from cardiopulmonary bypass (heart-lung bypass) machines used to perform open heart surgery. But ECMO equipment is optimised for support lasting days to weeks rather than hours.
xxxxxxxxxxxxxxxxx
Latest News Article Dated 17th Nov 2021:-
What is ECMO & why are doctors worried to see ICU patients being put on it for advanced life support?
ECMO, which stands for extra corporeal membrane oxygenation, is the life support of last resort for patients with severe heart and lung failure.
PTI
November 17, 2021, 18:20 IST

Doctors and health experts have expressed shock on social media recently about the number of ICU patients on ECMO treatment, especially in Victoria.
ECMO, which stands for extra corporeal membrane oxygenation, is the life support of last resort for patients with severe heart and lung failure.
At any one time, a busy ECMO hospital would normally have three to five patients supported with ECMO. The number of patients on ECMO at the Alfred Hospital in Melbourne is hovering around 20, almost all because of COVID.
In the US, hospitals report more requests for ECMO for teenagers and young adults and severely stretched resources.
xxxxxxxxxxxxxxxx
19th Nov 2021:
I wrote: I am a Physics and Numbers Man and never liked Chemistry. Can you explain how we Inhale air and how the blood gets oxygenated and CO2 Exhaled every breath we take. I know the veins deliver oxygen depleted blood to the Upper chambers of the heart that gets pumped by the heart muscles to the lower chamber on to the lungs where it gets oxygenated and returned to a third chamber and up to the fourth where the higher systolic pressure from the heart pushes oxygenated blood to the littlest capillary in all remote parts of the body. This is the mechanic that I understand which is almost like an IC Engine.
How is CO2 extracted and replaced by O2 is what I am trying to find out today. If you know please help me out
xxxxxxxxxxxxxx
Blood enters the right atrium and passes through the right ventricle. The right ventricle pumps the blood to the lungs where it becomes oxygenated. The oxygenated blood is brought back to the heart by the pulmonary veins which enter the left atrium. From the left atrium blood flows into the left ventricle.
As the ventricle contracts, blood leaves the heart through the pulmonic valve, into the pulmonary artery and to the lungs, where it is oxygenated. The oxygenated blood then returns to the heart through the pulmonary veins
In Other words - The right ventricle receives deoxygenated blood from the right atrium above, then pumps the blood along to the lungs to get oxygen. The left ventricle receives oxygenated blood from the left atrium, then sends it on to the aorta. The aorta branches into the systemic arterial network that supplies all of the body.
xxxxxxxxxxxxxxxx
The circulatory system (CCEA)
xxxxxxxxxxxxxxxx
Diffusion within RBCs
The rate at which RBCs can exchange oxygen and carbon dioxide is a measure of the fitness of the cells. In order to exchange gases, the cells undergo a number of steps including gas permeation across the cell membrane and hemoglobin binding. In the case of CO2, the molecules are converted to HCO3- ions and H+ ions.
The HCO3- ions are transported by the anion exchanger, AE1, and the H+ ions are buffered by hemoglobin. Cytoplasmic diffusion within the cell links all of these processes. The efficiency of gas exchange depends on protein-facilitated membrane transport, including transport of HCO3- ions by AE1 and membrane protein-assisted gas permeation.
The flattened shape of RBCs is believed to facilitate gas exchange by increasing the surface area to volume ratio and reducing the path-length for cytoplasmic diffusion, and thereby reducing delays introduced by cytoplasmic diffusion. However, these advantages have been found to be modest.
Sources:
Hemoglobin diffusion and the dynamics of oxygen capture by red blood cells
Steady state diffusion of oxygen in red blood cell and model suspensions
Exchange diffusion in human red blood cells
Hemoglobin
How does oxygen get to muscles?
Red blood cell thickness is evolutionarily constrained by slow, hemoglobin-restricted diffusion in cytoplasm
Further Reading
All Cellular Biology Content
Structure and Function of the Cell Nucleus
What Are Organelles?
Ribosome Structure
Protein Production: Initiation, Elongation and Termination
More...
Last Updated: Feb 26, 2019
xxxxxxxxxxxxxxxx
Understanding Human Autonomic System
What is autonomic function?
The autonomic system is the part of the peripheral nervous system that is responsible for regulating involuntary body functions, such as heartbeat, blood flow, breathing, and digestion
What is autonomic system?
The autonomic nervous system is a component of the peripheral nervous system that regulates involuntary physiologic processes including heart rate, blood pressure, respiration, digestion, and sexual arousal. It contains three anatomically distinct divisions: sympathetic, parasympathetic, and enteric
There is only one autonomous (or autonomic) nervous system.
What is difference between sympathetic and parasympathetic?
The sympathetic nervous system is involved in preparing the body for stress-related activities; the parasympathetic nervous system is associated with returning the body to routine, day-to-day operations. The two systems have complementary functions, operating in tandem to maintain the body's homeostasis.
In what ways does the human body function autonomously?
The autonomic nervous system regulates certain body processes, such as blood pressure and the rate of breathing. This system works automatically (autonomously), without a person's conscious effort. Disorders of the autonomic nervous system can affect any body part or process.
xxxxxxxxxxxxxx
If you have any valuable suggestions kindly drop me a note
My Assumption:
Engineers and Technologists are the Brains behind each and every medical gadget that gets used in this century.
Burnstein was an Electrical Engineer born with Type1 diabetes and almost lost his life several times due to Diabetic Hypoglycemia & Keto acidosis and wanted to take charge of his diabetes and stay alive. When the Going gets tough, the Tough get Gpoing, so he decided to study medicine and became an Endocrinologist too as a Mature age student and he battled with FDA to allow Patients to Monitor Blood sugar levels at home using little portable machine with strips. The Medical Profession was dead against it.
In 2021 a patient who is a Diabetic Type 1 or Type 1.5 of Type 2 will be considered stupid for not monitoring BSLs at home on a daly basis unless you are too poor to afford one. Not to forget the insulin pump that Mithu uses that takes the guess work out of both doctors and patients
When my Mother suffered a Brain stem stroke all they had in India was X Ray & Basic CT Machines. My Good Fortune I have CT Scans with and without Contrasts, Ultra sound machines, MRI and MRA and then we have PET scans and what not.
Today we have hearing aids that are programmable for various situations like Restaurants, Theatres, TV and Computers using Blue Tooth.
Yes I am aware of ECMO too and that was designed to serve lung cancer patients post surgery and prohibitive in Cost and cannot be used for not too long.
I lost a Very Very Good Friend in Bangalore Hospital.
He whatsapped me on a Wednesday with a non descript message. Went into a Hospital for a Heart Valve Replacement, which he did not tell me about, as he probably assumed it was simple and straight forward. Surgery was successful but he the Pateient died in ICU Post Surgery as he could not cope with ECMO. This is Just one story
So Why not study this problem and see why it is not possible to Oxygenate the Blood using a drip or some other means bypassing the lungs?
Responses:
Dr.Surbhi Vaish AIIMs:
Sure.. Ram Da. What you say has many truths to it. Let me get back to you on this in depth
Er. Raju Jairam:
Dai, heart-lung machines are used in surgery but not in long term oxygenation of blood. Certain surgeries require intubation when the patient doesn’t have enough lung capacity. You could pump blood through an artificial lung, but you’ll be anchored to the device.
People also use iron lungs and hyperbaric chambers, where again it is a cumbersome / immovable device.
There are some alternate masks which are shaped like a dome that fits over your entire head. There has been some success with that device. In any event you’d want to get the patient breathing on her/his own as quickly as possible.
I agree that intubation is a very aggressive procedure and can cause LT damage.
The primary focus is to reduce and eventually remove the gunk in the lungs and keep them operational. In the meantime the patient needs supplemental oxygenation of blood.
Er. Shankar Swamy:
Ram, I understand, from my Doctor friends, that ECMO does that. It's done during Bypass surgery etc
Just like dialysis, he says
Here is a Recent Article:-
xxxxxxxxxxxxxxxxxx
Er. Chandra Kumar :
valid question....have no idea....ECMO is used to rest lungs and heart during surgeries...thats high end. what is needed is a low cost ECMO where there is no need for surgery
Extracorporeal Membrane Oxygenation (ECMO)
https://www.ucsfhealth.org/treatments/extracorporeal-membrane-oxygenation
ECMO stands for extracorporeal membrane oxygenation. The ECMO machine is similar to the heart-lung by-pass machine used in open-heart surgery. It pumps and oxygenates a patient's blood outside the body, allowing the heart and lungs to rest. When you are connected to an ECMO, blood flows through tubing to an artificial lung in the machine that adds oxygen and takes out carbon dioxide; then the blood is warmed to body temperature and pumped back into your body.
There are two types of ECMO.
When my Mother suffered a Brain stem stroke all they had in India was X Ray & Basic CT Machines. My Good Fortune I have CT Scans with and without Contrasts, Ultra sound machines, MRI and MRA and then we have PET scans and what not.
Today we have hearing aids that are programmable for various situations like Restaurants, Theatres, TV and Computers using Blue Tooth.
Yes I am aware of ECMO too and that was designed to serve lung cancer patients post surgery and prohibitive in Cost and cannot be used for not too long.
I lost a Very Very Good Friend in Bangalore Hospital.
He whatsapped me on a Wednesday with a non descript message. Went into a Hospital for a Heart Valve Replacement, which he did not tell me about, as he probably assumed it was simple and straight forward. Surgery was successful but he the Pateient died in ICU Post Surgery as he could not cope with ECMO. This is Just one story
So Why not study this problem and see why it is not possible to Oxygenate the Blood using a drip or some other means bypassing the lungs?
Responses:
Dr.Surbhi Vaish AIIMs:
Sure.. Ram Da. What you say has many truths to it. Let me get back to you on this in depth
Er. Raju Jairam:
Dai, heart-lung machines are used in surgery but not in long term oxygenation of blood. Certain surgeries require intubation when the patient doesn’t have enough lung capacity. You could pump blood through an artificial lung, but you’ll be anchored to the device.
People also use iron lungs and hyperbaric chambers, where again it is a cumbersome / immovable device.
There are some alternate masks which are shaped like a dome that fits over your entire head. There has been some success with that device. In any event you’d want to get the patient breathing on her/his own as quickly as possible.
I agree that intubation is a very aggressive procedure and can cause LT damage.
The primary focus is to reduce and eventually remove the gunk in the lungs and keep them operational. In the meantime the patient needs supplemental oxygenation of blood.
Er. Shankar Swamy:
Ram, I understand, from my Doctor friends, that ECMO does that. It's done during Bypass surgery etc
Just like dialysis, he says
Here is a Recent Article:-
xxxxxxxxxxxxxxxxxx
Er. Chandra Kumar :
valid question....have no idea....ECMO is used to rest lungs and heart during surgeries...thats high end. what is needed is a low cost ECMO where there is no need for surgery
Extracorporeal Membrane Oxygenation (ECMO)
https://www.ucsfhealth.org/treatments/extracorporeal-membrane-oxygenation
ECMO stands for extracorporeal membrane oxygenation. The ECMO machine is similar to the heart-lung by-pass machine used in open-heart surgery. It pumps and oxygenates a patient's blood outside the body, allowing the heart and lungs to rest. When you are connected to an ECMO, blood flows through tubing to an artificial lung in the machine that adds oxygen and takes out carbon dioxide; then the blood is warmed to body temperature and pumped back into your body.
There are two types of ECMO.
The VA ECMO is connected to both a vein and an artery and is used when there are problems with both the heart and lungs. The VV ECMO is connected to one or more veins, usually near the heart, and is used when the problem is only in the lungs.
USCF is also now using a smaller portable ECMO device that is light enough to be carried by one person and can be transported in an ambulance or helicopter, making it possible to provide ECMO relief in emergency cases.
When is ECMO used:
For patients recovering from heart failure, or lung failure or heart surgery.
As a bridge option to further treatment, when doctors want to assess the state of other organs such as the kidneys or brain before performing heart or lung surgery.
USCF is also now using a smaller portable ECMO device that is light enough to be carried by one person and can be transported in an ambulance or helicopter, making it possible to provide ECMO relief in emergency cases.
When is ECMO used:
For patients recovering from heart failure, or lung failure or heart surgery.
As a bridge option to further treatment, when doctors want to assess the state of other organs such as the kidneys or brain before performing heart or lung surgery.
For support during high-risk procedures in the cardiac catheterization lab.
As a bridge to a heart assist device, such as left ventricular assist device (LVAD).
As a bridge for patients awaiting lung transplant. The ECMO helps keep tissues well oxygenated, which makes the patient a better candidate for transplant.
Procedure
Being placed on ECMO requires a surgical procedure but it is usually done in a patient's room. The patient is sedated and given pain medication and an anti-coagulant to minimize blood clotting. A surgeon, assisted by an operating room team, inserts the ECMO catheters into either an artery or veins. An x-ray is then taken to ensure the tubes are in the right place. Usually a patient on the ECMO pump will also be on a ventilator, which helps the lungs to heal. While on ECMO, the patient will be monitored by specially trained nurses and respiratory therapists, as well as the surgeon and surgical team. Since you will be sedated and have a breathing tube in place, supplemental nutrition will be provided either intravenously or though a nasal-gastric tube. Nutrition is delivered either intravenously or though a nasal-gastric tube
While on ECMO, you may be given certain medications including: heparin to prevent blood clots; antibiotics to prevent infections; sedatives to minimize movement and improve sleep; diuretics to help the kidney get rid of fluids; electrolytes to maintain the proper balance of salts and sugars; and blood products to replace blood loss.
Discontinuing ECMO requires a surgical procedure to remove the tubes. Multiple tests are usually done prior to the discontinuation of ECMO therapy to confirm that your heart and lungs are ready. Once the ECMO cannulas are removed, the vessels will need to be repaired. This can be done either at the bedside or in the operating room. The doctor will use small stitches to close the spot where the tubes were placed. You will be asleep and monitored for this process. Even though you are off the ECMO, you may still need to be on a ventilator.
Risks
ECMO does carry risks including:
Bleeding, due to the medication that's given to prevent blood from clotting in the tubing.
Infection at the sites where the tubes enter the body.
Transfusion problems, since a person on ECMO is given blood products.
Small clots or air bubbles forming in the tubing.
Increased chance of stroke.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
xxxxxxxxxxxxxxx
Er. Mutharasan:
External oxygenation via Heart-Lung Machine is OK for short time, such as a few hours. Long time usage will introduce other complications. Besides it is an expensive procedure.
xxxxxxxxxxxxxxxxx
Er. Nacha:
There is a procedure called ECMO which stands for ExtraCorporeal Membrane Oxygenation but these are for extreme cases.
xxxxxxxxxxxxxxxxx
Er. Chiku Machayya:-
This is an excellent question. I don't have a solid answer right now. One reason I can think of is that the blood contains iron salts which naturally absorb oxygen. A depletion of these salts reduces it's oxygen carrying capacity. However, outside the lung there may be other reasons why the blood does not absorb oxygen as easily. It takes time, and by the time the oxygen is sent back to the patient, it may be too late.
Risks
ECMO does carry risks including:
Bleeding, due to the medication that's given to prevent blood from clotting in the tubing.
Infection at the sites where the tubes enter the body.
Transfusion problems, since a person on ECMO is given blood products.
Small clots or air bubbles forming in the tubing.
Increased chance of stroke.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
xxxxxxxxxxxxxxx
Er. Mutharasan:
External oxygenation via Heart-Lung Machine is OK for short time, such as a few hours. Long time usage will introduce other complications. Besides it is an expensive procedure.
xxxxxxxxxxxxxxxxx
Er. Nacha:
There is a procedure called ECMO which stands for ExtraCorporeal Membrane Oxygenation but these are for extreme cases.
xxxxxxxxxxxxxxxxx
Er. Chiku Machayya:-
This is an excellent question. I don't have a solid answer right now. One reason I can think of is that the blood contains iron salts which naturally absorb oxygen. A depletion of these salts reduces it's oxygen carrying capacity. However, outside the lung there may be other reasons why the blood does not absorb oxygen as easily. It takes time, and by the time the oxygen is sent back to the patient, it may be too late.
xxxxxxxxxxxxxxxxx
Dr.Sachitra - Sydney
Uncle sorry dint get time to reply...had me thinking...
Coz in my field i know intubation only has saved so many lives... Yes it has its downfall and disadvantages especially if u don't know how to ventilate, but now a days the understanding is so much better regarding all this.
There is a way where we can oxygenate outside which is called ECMO...its so expensive. Even in countries like ours there are certain indicators when u can put on ecmo
xxxxxxxxxx
Er. Manju Gupta
Regarding your Research Topic on oxygen intubation, yes I wholly agree that such practice can suffocate a patient. Agree that such infusion of oxygen rich blood after having been thru a enrichment process would benefit a patient.
After the patient is dead we cannot carry out a enquiry to ask him if he felt difficulty in breathing once a tube is pushed down his throat.
Technically this plasma or hameoglobin enrichment process is feasible - only such research to invent a machine is necessary , like dialysis .
Good thinking . Manju
xxxxxxxx
Dr.Manjula Krishnaswamy ( My surgeon Sister)
The process of oxygenation is a complex process of the haem molecule exchanging gases which happens in the lung. It is not simple diffusion of oxygen into the blood / plasma. It's only haemoglobin in the blood that carries oxygen or cabondioxide
xxxxxxxxxxxxx
Er. Anand Rangarajan:
This machine is called the heart/lung machine. It’s just too expensive to implement
xxxxxxxxxxxxxx
Amaresh Simhadri :
I don't have a suggestion but it's a good topic for research. On this why do you think none of the scientist didn't think of it,?
xxxxxxxxxxxxxx
Er. Prof Ranganathan
Rambo, oxygenating the blood bypassing the lungs- If only we had shown this level of interest in our IIT days, to our subjects, we would have become Einsteins. One of my senior Professors used to say,. "We are always experts in some one else's subject' ! "
Now on the topic at hand, plants breathe in co2 and breathe out oxygen. So why nor eat and digest live plants like animals do ? Or separate water, H2O, and take out hydrogen and leave the rest in the body.
This is in consonance with our policy of thinking solar energy is coming at zero cost because sun is free.
(Great Response. Have to check out how Oxygen for medical use is Manufactured)
xxxxxxxxxxxxxx
Er. Ashley Solomon
I seem to recall data showing that intubation is a traumatic procedure that rarely saves lives. Your idea to oxygenated the blood directly is elegant. One would think it would have been tried already or at least investigated.
xxxxxxxxxxx
Blood Oximeter for measuring Blood Oxygen Saturation Levels
xxxxxxxxxxxx
My Initial Findings Just now :- 18th Nov 2021
I PLAN TO DIG DEEP

In Association with ETHealthworld
My Initial Findings Just now :- 18th Nov 2021
I PLAN TO DIG DEEP

In Association with ETHealthworld
Parexel India Symposium
25 November 2021 @ 05:00 PM
Virtual Event





Register Now
ECMO is a vital tool but it requires highly trained staff and a huge amount of hospital resources. Patients who survive ECMO support may have long term health complications related to their critical illness.
Outsourcing the heart and lungs
In lay terms, ECMO is a heart or lung bypass machine. A pump and artificial lung, both sitting outside the body, provide a level of support the sick organs can no longer provide. This way, the rest of the body's functions are maintained.
The meaning of each of the letters of the ECMO acronym is:
Extra Corporeal: outside the body
Membrane: the artificial lung is referred to as a “membrane”, or thin layer of material that keeps blood flowing on one side and oxygen on the other. This thin and porous membrane allows oxygen in and carbon dioxide out
Oxygenation: when oxygen enters the blood it is equivalent to breathing in. The process equivalent to breathing out, the removal of carbon dioxide, also occurs.
As well as the oxygenator, the ECMO machine includes cannulae – or tubing – to drain the blood from the patient and return it once oxygen has been added and carbon dioxide removed, a pump and a control panel.
ECMO evolved from cardiopulmonary bypass (heart-lung bypass) machines used to perform open heart surgery. But ECMO equipment is optimised for support lasting days to weeks rather than hours.
xxxxxxxxxxxxxxxxx
Latest News Article Dated 17th Nov 2021:-
What is ECMO & why are doctors worried to see ICU patients being put on it for advanced life support?
ECMO, which stands for extra corporeal membrane oxygenation, is the life support of last resort for patients with severe heart and lung failure.
PTI
November 17, 2021, 18:20 IST

Doctors and health experts have expressed shock on social media recently about the number of ICU patients on ECMO treatment, especially in Victoria.
ECMO, which stands for extra corporeal membrane oxygenation, is the life support of last resort for patients with severe heart and lung failure.
At any one time, a busy ECMO hospital would normally have three to five patients supported with ECMO. The number of patients on ECMO at the Alfred Hospital in Melbourne is hovering around 20, almost all because of COVID.
In the US, hospitals report more requests for ECMO for teenagers and young adults and severely stretched resources.
xxxxxxxxxxxxxxxx
19th Nov 2021:
I wrote: I am a Physics and Numbers Man and never liked Chemistry. Can you explain how we Inhale air and how the blood gets oxygenated and CO2 Exhaled every breath we take. I know the veins deliver oxygen depleted blood to the Upper chambers of the heart that gets pumped by the heart muscles to the lower chamber on to the lungs where it gets oxygenated and returned to a third chamber and up to the fourth where the higher systolic pressure from the heart pushes oxygenated blood to the littlest capillary in all remote parts of the body. This is the mechanic that I understand which is almost like an IC Engine.
How is CO2 extracted and replaced by O2 is what I am trying to find out today. If you know please help me out
xxxxxxxxxxxxxx
Blood enters the right atrium and passes through the right ventricle. The right ventricle pumps the blood to the lungs where it becomes oxygenated. The oxygenated blood is brought back to the heart by the pulmonary veins which enter the left atrium. From the left atrium blood flows into the left ventricle.
As the ventricle contracts, blood leaves the heart through the pulmonic valve, into the pulmonary artery and to the lungs, where it is oxygenated. The oxygenated blood then returns to the heart through the pulmonary veins
In Other words - The right ventricle receives deoxygenated blood from the right atrium above, then pumps the blood along to the lungs to get oxygen. The left ventricle receives oxygenated blood from the left atrium, then sends it on to the aorta. The aorta branches into the systemic arterial network that supplies all of the body.
xxxxxxxxxxxxxxxx
The circulatory system (CCEA)
Blood is pumped away from the heart at high pressure in arteries, and returns to the heart at low pressure in veins. The human circulatory system is a double circulatory system.
The heart
The heart is a unidirectional pump.
Valves are present to prevent the backflow of blood.
The right side pumps deoxygenated blood (low in oxygen and high in carbon dioxide) to the lungs.
The left side pumps oxygenated blood (high in oxygen and low in carbon dioxide) to the organs of the body.
Deoxygenated blood enters the right atrium from the vena cava.
Blood moves into right ventricle.
Blood is pumped into the pulmonary artery.
The pulmonary artery carries deoxygenated blood to the lungs.
The blood becomes oxygenated in the lungs.
Oxygenated blood leaves the lung via the pulmonary vein.
Blood enters the left atrium.
Blood moves into the left ventricle.
Blood is pumped into the aorta, which carries oxygenated blood around the body.
This unidirectional flow of blood through the heart shows that mammals have a double circulatory system.This means blood travels through the heart twice in one circulation of the body.
![]()
Ventricular walls are thicker than atrial walls because the ventricles have to pump blood further.
The left ventricle wall is thicker than the right because it pumps blood around the body while the right pumps blood to the lungs, located close to the heart.
The following arteries and veins transport blood to and from some of the body’s organs:
Blood vesselFunction Vena cava Carries deoxygenated blood from the body back to the heart.
Pulmonary artery Carries deoxygenated blood from the heart to the lungs.
Pulmonary vein Carries oxygenated blood from the lungs to the heart.
Aorta Carries oxygenated blood from the heart around the body.
Hepatic artery Carries oxygenated blood to the liver.
Hepatic vein Carries deoxygenated blood back to the heart. Carries digested food (glucose and amino acids) from the liver around the body.
Hepatic portal vein Carries digested food from the small intestine to the liver.
Renal artery Carries oxygenated blood (also rich in urea) to the kidneys for excretion.
Renal vein Carries deoxygenated blood (also low in urea as it has been purified in the kidney) back to the heart.
The oxygen and glucose carried in oxygenated blood is used for respiration in the body’s cells.The coronary arteries provide the heart muscle with the glucose and oxygen it needs for respiration.
These are small blood vessels that branch off the aorta and can be seen on the external surface of the heart.
The heart
The heart is a unidirectional pump.
Valves are present to prevent the backflow of blood.
The right side pumps deoxygenated blood (low in oxygen and high in carbon dioxide) to the lungs.
The left side pumps oxygenated blood (high in oxygen and low in carbon dioxide) to the organs of the body.
Deoxygenated blood enters the right atrium from the vena cava.
Blood moves into right ventricle.
Blood is pumped into the pulmonary artery.
The pulmonary artery carries deoxygenated blood to the lungs.
The blood becomes oxygenated in the lungs.
Oxygenated blood leaves the lung via the pulmonary vein.
Blood enters the left atrium.
Blood moves into the left ventricle.
Blood is pumped into the aorta, which carries oxygenated blood around the body.
This unidirectional flow of blood through the heart shows that mammals have a double circulatory system.This means blood travels through the heart twice in one circulation of the body.
Ventricular walls are thicker than atrial walls because the ventricles have to pump blood further.
The left ventricle wall is thicker than the right because it pumps blood around the body while the right pumps blood to the lungs, located close to the heart.
The following arteries and veins transport blood to and from some of the body’s organs:
Blood vesselFunction Vena cava Carries deoxygenated blood from the body back to the heart.
Pulmonary artery Carries deoxygenated blood from the heart to the lungs.
Pulmonary vein Carries oxygenated blood from the lungs to the heart.
Aorta Carries oxygenated blood from the heart around the body.
Hepatic artery Carries oxygenated blood to the liver.
Hepatic vein Carries deoxygenated blood back to the heart. Carries digested food (glucose and amino acids) from the liver around the body.
Hepatic portal vein Carries digested food from the small intestine to the liver.
Renal artery Carries oxygenated blood (also rich in urea) to the kidneys for excretion.
Renal vein Carries deoxygenated blood (also low in urea as it has been purified in the kidney) back to the heart.
The oxygen and glucose carried in oxygenated blood is used for respiration in the body’s cells.The coronary arteries provide the heart muscle with the glucose and oxygen it needs for respiration.
These are small blood vessels that branch off the aorta and can be seen on the external surface of the heart.
xxxxxxxxxxxxxxxx
Red blood cells pick up oxygen in the lungs. Blood travels away from the heart and lungs through the arteries. Red blood cells drop off oxygen to the cells through tiny tubes called capillaries. Blood then returns to the heart
Red blood cells pick up oxygen in the lungs. Blood travels away from the heart and lungs through the arteries. Red blood cells drop off oxygen to the cells through tiny tubes called capillaries. Blood then returns to the heart
xxxxxxxxxxxxxxxx
Bradi Cardia - That almost killed me as my Quack Cardiologist kept insisting for 12 long years that my symptoms were all on my mind and echo done four times a year shows my heart was in good nick and what I was experiencing was Exercise Induced asthma ( A Load of BS)In Jan 2017 my Pulse rate was dropping to below 50 and my Blood oxygen levels down to 93% and I was struggling to even walk to my car. I put up a Fight with the man and Insisted on HOLTER Monitor which he again delayed for a week. The following evening he looks at the results and tells my wife OMG he needs a Pace Maker immediately and Off to hospital emergency. The surgeon who implanted the Pace maker tells my son "Your Dad is Lucky as his is stage three Bardicardia and a few more days he would have died".
So How did my Cardiologist miss it? He relied on Echo Cardiogram and stress test and was not listening to patients complaints for years. Plus he was using an obsolete ECG Machine which did not pick up BradiCardia. This is why I say don't Have Blind Belief and Trust in your Doctors. It is your life so Take Charge. I gave the Quack the Flick straight away when I realised he did not know anything about my sophisticated Pace Maker that cost Aud $25K. Not happy with your doctor find some one who you feel is a Good caring Physician
So How did my Cardiologist miss it? He relied on Echo Cardiogram and stress test and was not listening to patients complaints for years. Plus he was using an obsolete ECG Machine which did not pick up BradiCardia. This is why I say don't Have Blind Belief and Trust in your Doctors. It is your life so Take Charge. I gave the Quack the Flick straight away when I realised he did not know anything about my sophisticated Pace Maker that cost Aud $25K. Not happy with your doctor find some one who you feel is a Good caring Physician
xxxxxxxxxxxxxxxx
How does oxygen get into the bloodstream?
Inside the air sacs, oxygen moves across paper-thin walls to tiny blood vessels called capillaries and into your blood. A protein called haemoglobin in the red blood cells then carries the oxygen around your body. At the same time, carbon dioxide that is dissolved in the blood comes out of the capillaries back into the air sacs, ready to be breathed out.

Blood with fresh oxygen is carried from your lungs to the left side of your heart, which pumps blood around your body through the arteries.
Blood without oxygen returns through the veins, to the right side of your heart. From there it is pumped to your lungs so that you can breathe out the carbon dioxide and breathe in more oxygen.
xxxxxxxxxxxxxxxx
A protein called haemoglobin in the red blood cells then carries the oxygen around your body
So Haemoglobin cells absorb Oxygen from air sacs in the lung and also expels CO2 which the Lung exhales
xxxxxxxxxxxxxxx
As an Engineer I am Thinking haemoglobin cells in the Blood will absorb oxygen from any source and not necessarily the Lungs. and co2 can be exhaled through the lungs
I am not thinking of Non functioning Lungs as in lung cancer as the Lungs are Kaput
The ECMO as we know it was designed and developed to assist Lung and heart patients Post major surgery like Transplant.
My Search is to find out howe to keep he blood oxygenated outside the lungs to support weak and ailing lungs. I see no point putting oxygen under pressure into a weak diseased Lung.
There has to be a way. Blood absorbs every damn thing we inject into it with needles and drips be it insulin or antibiotics, iron, plasma, Platelets and what not.
My assumption is If the Blood is Oxygenated the Body is healthier. Replace Oxygen with Nitrogen as happened to my cousin and it killed her
xxxxxxx
Listen to this :-
How does oxygen enter a red blood cell from the alveoli
In a process called diffusion, oxygen moves from the alveoli to the blood through the capillaries (tiny blood vessels) lining the alveolar walls.
Once in the bloodstream, oxygen gets picked up by the hemoglobin in red blood cells.
This is the Key to what I was looking for. Once Oxygen is introduced into the blood stream the haemoglobin cells absorb the oxygen.
Inside the air sacs, oxygen moves across paper-thin walls to tiny blood vessels called capillaries and into your blood. A protein called haemoglobin in the red blood cells then carries the oxygen around your body. At the same time, carbon dioxide that is dissolved in the blood comes out of the capillaries back into the air sacs, ready to be breathed out.

Blood with fresh oxygen is carried from your lungs to the left side of your heart, which pumps blood around your body through the arteries.
Blood without oxygen returns through the veins, to the right side of your heart. From there it is pumped to your lungs so that you can breathe out the carbon dioxide and breathe in more oxygen.
xxxxxxxxxxxxxxxx
A protein called haemoglobin in the red blood cells then carries the oxygen around your body
So Haemoglobin cells absorb Oxygen from air sacs in the lung and also expels CO2 which the Lung exhales
xxxxxxxxxxxxxxx
As an Engineer I am Thinking haemoglobin cells in the Blood will absorb oxygen from any source and not necessarily the Lungs. and co2 can be exhaled through the lungs
I am not thinking of Non functioning Lungs as in lung cancer as the Lungs are Kaput
The ECMO as we know it was designed and developed to assist Lung and heart patients Post major surgery like Transplant.
My Search is to find out howe to keep he blood oxygenated outside the lungs to support weak and ailing lungs. I see no point putting oxygen under pressure into a weak diseased Lung.
There has to be a way. Blood absorbs every damn thing we inject into it with needles and drips be it insulin or antibiotics, iron, plasma, Platelets and what not.
My assumption is If the Blood is Oxygenated the Body is healthier. Replace Oxygen with Nitrogen as happened to my cousin and it killed her
xxxxxxx
Listen to this :-
How does oxygen enter a red blood cell from the alveoli
In a process called diffusion, oxygen moves from the alveoli to the blood through the capillaries (tiny blood vessels) lining the alveolar walls.
Once in the bloodstream, oxygen gets picked up by the hemoglobin in red blood cells.
This is the Key to what I was looking for. Once Oxygen is introduced into the blood stream the haemoglobin cells absorb the oxygen.
xxxxxxxxxxxxxxx
Diffusion and Red Blood Cells
Download PDF Copy

By Dr. Catherine Shaffer, Ph.D.
Reviewed by Chloe Barnett, BSc
Animals breathe in oxygen, following which it must be delivered to all the organs in the body. This process involves red blood cells and diffusion.
Red blood cells
Red blood cells (RBCs) are a type of blood cell whose role is to transport oxygen from the lungs to the peripheral tissues of the body. Oxygen diffuses from the alveoli of the lungs into the RBCs, where it binds to hemoglobin. One molecule of hemoglobin can bind four molecules of oxygen (O2).
The partial pressure of oxygen determines the affinity of hemoglobin for oxygen. In the lungs, the partial pressure of oxygen is high, and hemoglobin has a high affinity for oxygen. In other tissues, the partial pressure of oxygen is lower, and hemoglobin releases its oxygen molecules.
This difference in affinities is important for oxygen to be delivered where it’s needed. Red blood cells have the shape of a flattened disk, generating a broad surface area for the diffusion of oxygen. Since their only purpose is carrying oxygen throughout the body, they lack many typical cell structures, including a nucleus.
Hemoglobin
Related Stories
Gelatin hydrogel can be used in trophoblast spheroid motility assays, shows study
New evidence reveals a cancer-promoting role for MAPK6 enzyme
Biomedical engineer receives NASA grant to find ways to keep astronauts' bones strong in space
Red blood cells are filled with hemoglobin. Hemoglobin is a globular protein comprised of four polypeptide chains with an iron-binding group called heme on each chain. The heme group has affinity for oxygen and when oxygen is present it is red, but when it lacks oxygen it is bluish. Hemoglobin also binds waste carbon dioxide for its return to the lungs, but this does not occur at its heme binding site.
Fetal hemoglobin
A developing fetus receives oxygen through the mother’s blood supply. Fetal hemoglobin has a higher affinity for oxygen than maternal blood, in order for oxygen to be successfully transferred from maternal red blood cells through the placenta to fetal red blood cells.
The reason that fetal hemoglobin has a greater affinity for oxygen is that it lacks an ability to interact with 2,3-bisphosphoglycerate (2,3-BPG), which in adult cells reduces the affinity for oxygen. The difference is due to a single amino acid change in the 2,3-BPG binding pocket.
Diffusion and Red Blood Cells
Download PDF Copy

By Dr. Catherine Shaffer, Ph.D.
Reviewed by Chloe Barnett, BSc
Animals breathe in oxygen, following which it must be delivered to all the organs in the body. This process involves red blood cells and diffusion.
Credit: eyeretina/Shuttertstock.com
Red blood cells (RBCs) are a type of blood cell whose role is to transport oxygen from the lungs to the peripheral tissues of the body. Oxygen diffuses from the alveoli of the lungs into the RBCs, where it binds to hemoglobin. One molecule of hemoglobin can bind four molecules of oxygen (O2).
The partial pressure of oxygen determines the affinity of hemoglobin for oxygen. In the lungs, the partial pressure of oxygen is high, and hemoglobin has a high affinity for oxygen. In other tissues, the partial pressure of oxygen is lower, and hemoglobin releases its oxygen molecules.
This difference in affinities is important for oxygen to be delivered where it’s needed. Red blood cells have the shape of a flattened disk, generating a broad surface area for the diffusion of oxygen. Since their only purpose is carrying oxygen throughout the body, they lack many typical cell structures, including a nucleus.
Hemoglobin
Related Stories
Gelatin hydrogel can be used in trophoblast spheroid motility assays, shows study
New evidence reveals a cancer-promoting role for MAPK6 enzyme
Biomedical engineer receives NASA grant to find ways to keep astronauts' bones strong in space
Red blood cells are filled with hemoglobin. Hemoglobin is a globular protein comprised of four polypeptide chains with an iron-binding group called heme on each chain. The heme group has affinity for oxygen and when oxygen is present it is red, but when it lacks oxygen it is bluish. Hemoglobin also binds waste carbon dioxide for its return to the lungs, but this does not occur at its heme binding site.
Fetal hemoglobin
A developing fetus receives oxygen through the mother’s blood supply. Fetal hemoglobin has a higher affinity for oxygen than maternal blood, in order for oxygen to be successfully transferred from maternal red blood cells through the placenta to fetal red blood cells.
The reason that fetal hemoglobin has a greater affinity for oxygen is that it lacks an ability to interact with 2,3-bisphosphoglycerate (2,3-BPG), which in adult cells reduces the affinity for oxygen. The difference is due to a single amino acid change in the 2,3-BPG binding pocket.
Diffusion within RBCs
The rate at which RBCs can exchange oxygen and carbon dioxide is a measure of the fitness of the cells. In order to exchange gases, the cells undergo a number of steps including gas permeation across the cell membrane and hemoglobin binding. In the case of CO2, the molecules are converted to HCO3- ions and H+ ions.
The HCO3- ions are transported by the anion exchanger, AE1, and the H+ ions are buffered by hemoglobin. Cytoplasmic diffusion within the cell links all of these processes. The efficiency of gas exchange depends on protein-facilitated membrane transport, including transport of HCO3- ions by AE1 and membrane protein-assisted gas permeation.
The flattened shape of RBCs is believed to facilitate gas exchange by increasing the surface area to volume ratio and reducing the path-length for cytoplasmic diffusion, and thereby reducing delays introduced by cytoplasmic diffusion. However, these advantages have been found to be modest.
Sources:
Hemoglobin diffusion and the dynamics of oxygen capture by red blood cells
Steady state diffusion of oxygen in red blood cell and model suspensions
Exchange diffusion in human red blood cells
Hemoglobin
How does oxygen get to muscles?
Red blood cell thickness is evolutionarily constrained by slow, hemoglobin-restricted diffusion in cytoplasm
Further Reading
All Cellular Biology Content
Structure and Function of the Cell Nucleus
What Are Organelles?
Ribosome Structure
Protein Production: Initiation, Elongation and Termination
More...
Last Updated: Feb 26, 2019
xxxxxxxxxxxxxxxx
Understanding Human Autonomic System
What is autonomic function?
The autonomic system is the part of the peripheral nervous system that is responsible for regulating involuntary body functions, such as heartbeat, blood flow, breathing, and digestion
What is autonomic system?
The autonomic nervous system is a component of the peripheral nervous system that regulates involuntary physiologic processes including heart rate, blood pressure, respiration, digestion, and sexual arousal. It contains three anatomically distinct divisions: sympathetic, parasympathetic, and enteric
There is only one autonomous (or autonomic) nervous system.
What is difference between sympathetic and parasympathetic?
The sympathetic nervous system is involved in preparing the body for stress-related activities; the parasympathetic nervous system is associated with returning the body to routine, day-to-day operations. The two systems have complementary functions, operating in tandem to maintain the body's homeostasis.
In what ways does the human body function autonomously?
The autonomic nervous system regulates certain body processes, such as blood pressure and the rate of breathing. This system works automatically (autonomously), without a person's conscious effort. Disorders of the autonomic nervous system can affect any body part or process.
xxxxxxxxxxxxxx
How is Oxygen Manufactured for medical use?
The benefits and hazards of liquid oxygen
Liquid oxygen therapy is the medical process of providing additional oxygen to patients
By Manas Ranjan Senapati
Published: Tuesday 13 July 2021

Liquid oxygen has a pale blue colour and is a cryogenic liquid. Cryogenic liquids are liquefied gases that have a normal boiling point below -238 degrees Fahrenheit (-150 degrees Celsius).
Oxygen is often stored as a liquid, although it is used primarily as a gas. The low temperature of liquid oxygen and the vapour it releases poses a serious burn hazard to human tissue. Materials which usually burn in ambient air will burn more vigorously in oxygen.
In commerce, liquid oxygen is classified as an industrial gas and is widely used for industrial and medical purposes. Liquid oxygen is used as an oxidant for liquid fuels in the propellant systems of missiles and rockets.
Oxygen is widely applied in the metal industries in conjunction with acetylene and other fuel gases for metal cutting, welding, hardening, cleaning and melting.
Liquid oxygen therapy is the medical process of providing additional oxygen to a patient who cannot get enough oxygen on their own. Conditions such as asthma, cystic fibrosis, dysphasia, chronic obstructive pulmonary disease, heart failure, lung disease and pneumonia can be treated by liquid oxygen
therapy.
Contact with liquid oxygen can cause severe skin and eye irritation and burns as well as frostbite. Normally, air contains 21 per cent oxygen and oxygen is essentially nontoxic.
No health effects have been observed in people exposed to concentrations up to 50 per cent liquid oxygen at one atmosphere pressure for 24 hours or longer. Inhalation of 80 per cent oxygen at one atmosphere for more than 12 hours can cause irritation of the respiratory tract, nausea, dizziness, muscle twitching, vision loss, coughing, nasal stuffiness, sore throat and chest pain.
A characteristic neurological syndrome can be observed when pure oxygen is inhaled at pressures greater than two or three atmospheres. Signs and symptoms include nausea, dizziness, vomiting, tiredness, light-headedness, mood changes, euphoria, confusion, incoordination, muscular twitching, burning / tingling sensations (particularly of the fingers and toes) and loss of consciousness.
Characteristic epilepsy-like convulsions, which may be preceded by visual disturbances such as loss of peripheral vision, also occur. Continued exposure can cause severe convulsions, leading to death. The effects are reversible after reduction of oxygen pressure.
The following are the hazards liquid oxygen is associated with:
No health effects have been observed in people exposed to concentrations up to 50 per cent liquid oxygen at one atmosphere pressure for 24 hours or longer. Inhalation of 80 per cent oxygen at one atmosphere for more than 12 hours can cause irritation of the respiratory tract, nausea, dizziness, muscle twitching, vision loss, coughing, nasal stuffiness, sore throat and chest pain.
A characteristic neurological syndrome can be observed when pure oxygen is inhaled at pressures greater than two or three atmospheres. Signs and symptoms include nausea, dizziness, vomiting, tiredness, light-headedness, mood changes, euphoria, confusion, incoordination, muscular twitching, burning / tingling sensations (particularly of the fingers and toes) and loss of consciousness.
Characteristic epilepsy-like convulsions, which may be preceded by visual disturbances such as loss of peripheral vision, also occur. Continued exposure can cause severe convulsions, leading to death. The effects are reversible after reduction of oxygen pressure.
The following are the hazards liquid oxygen is associated with:
Exposure to cold temperatures that can cause severe burns
Over pressurisation due to the expansion of small amounts of liquid into large volumes of gas in inadequately vented equipment
Oxygen enrichment of the surrounding atmosphere
The possibility of a combustion reaction if the oxygen is permitted to contact a noncompatible material.
Some common materials like asphalt, kerosene, cloth, wood, paint, tar and dirt containing oil or grease can react violently with liquid oxygen at certain pressures and temperatures.
Personnel must be thoroughly familiar with properties and safety considerations before being allowed to handle liquid oxygen and its associated equipment.
Views expressed are the author’s own and don’t necessarily reflect those of Down To Earth
HEALTH
I suffer from long COVID. Here is how I live without taste and smell
I also suffer from a host of other ailments that are among the 200 side-effects being endured by 100 million people who have recovered from COVID-19 globally
By Richard Mahapatra
Published: Thursday 18 November 2021

I have been living without two primordial senses for nearly 200 days now — smell and taste — and both are intimately connected. I tested positive for the novel coronavirus disease (COVID-19) towards the end of April this year, along with my wife and daughter.
As far as I remember, I lost my sense of taste and smell from the first week of May. As I write this, I have still not regained these two senses. Indeed, I am now almost reconciled to the scary possibility of living without them.
Or, it might just be a reconciliatory feeling that the long duration has instilled in me. Doctors have told me: “Have patience. It will come back.”
I reviewed many ‘inform yourself’ books that I collected when we were expecting our daughter. I just wanted to know whether the senses of taste and smell are biological or one develops them after birth.
This may sound like a foolish exploration for an existing biological being, but that is the level of frustration that this loss emotionally causes.
I am now assured that we are all born with five senses: Sight, hearing, smell, taste and touch. In fact, the nose forms in the first trimester of pregnancy and by 10 weeks, the baby, still in the womb, can smell things.
So, this is my first experience of living without smell and taste. And this experience answers another puzzling question for me: What happens if we lose taste and smell?
I am without two senses that primarily define our interface with the world, family, and the food that sustains us. I cook, but only enjoy it by deploying my pre-COVID memory of its taste and smell.
Stories and conversations on food are deliberately being re-told as we have dinner. So, I remember the specific taste and context of a dish that I consume. But physically, I just chew ‘things’, not being able to differentiate whether it is a piece of chicken or a fried piece of eggplant.
My appetite has reduced. I feel as if I am losing an ecosystem in which I grew up happy. In the vegetable market, I just do ‘shopping’. There is no more forensic evaluation of vegetables to ensure that particular taste and aroma in the final dish.
I have outsourced my senses to my wife and daughter — they taste and smell and remember my trademark dishes and give a verdict.
I just cook. There is no more of that indulgence that was an interface of social, biological and ecological things.
Every time I visited my home in Odisha, I came back with fresh chillies and lemons. They had a taste and aroma that bound me with my home and its ecology. They had a special, family-centric taste that I had imbibed in my memory. I consumed them to get that intimate connect and feel immense happiness. I can’t have that now.
It is just a memory, a clinical one. I am told the part of the brain that controls smell is also the one that controls memory. I don’t know if losing smell will lead to an altered memory as well.
Historians say without smell and taste, many colonisations wouldn’t have happened. For me, it could just be that I may find a disconnect with my kitchen, my most comfortable place at home where I hold India’s history and geography together in glass bottles.
A global emergency
In the six months since I tested positive for COVID-19, loss of taste and smell has been just one side-effect. Doctors have already listed 200 such effects that COVID-19 patients endure after recovery and those who endure any of them for more than a month, are being termed as suffering from ‘long COVID-19’.
I am undoubtedly a ‘long COVID’ patient. I have other side effects as well: Loss of hair; anxiety attacks, though they are less frequent now; a nagging brain fog; fatigue that has reduced by now but I still feel drained sometimes; pain in my lower legs; a dry skin condition and infrequent bouts of palpitations.
As of November 18, there are over 230 million COVID-19 recovered people in the world, just like me. The fight against the pandemic continues, but there is an increasing focus on the recovered population enduring long COVID-19. Such a significant population group has been sick with 200 types of side-effects for months. It is a medical, economical and social emergency, almost.
In a recent research (not peer reviewed), researchers from the University of Michigan estimated that 100 million of COVID-19 recovered people globally have been enduring long COVID-19. The researchers reviewed 40 studies from 17 countries on lingering side effects of COVID-19 to come to this conclusion.
They estimated that 40 per cent of the COVID-19 survivors suffer from the side-effects. The rate increases to 57 per cent for those who were hospitalised for COVID-19 treatment.
More women than men have long COVID-19: The University of Michigan study finds that 49 per cent of the recovered women patients have long COVID while it is 37 per cent for men.
The long COVID-19 is proportionate to the new infection cases. The more new cases pop up — the pandemic is still raging and Europe is currently witnessing a resurgence — the size of the recovered population group will also increase.
It means the probability of more people enduring long COVID-19 also increases. In the process, we will have a scenario when the world has more long COVID patients than those getting the infection fresh. And, at this point of time, the world health response will be just for this.
Richard Mahapatra is Managing Editor, Down To Earth
xxxxxxxxxxxxxxxxxxx
How About This Find ???
Wonder Foods Liquid Oxygen
Brand: Wonder Foods
$20.35 – $38.20 (-15%)
This unique supplement is super-charged with bioavailable oxygen that is easily absorbed by the body, making it immediately available at a cellular level.
Increasing energy and vitality
Sharper mental focus
Maintaining a healthy acid/alkaline balance
Size: 500ml Clear
$38.20 $44.95
( Looks like a Hoax promoted by Snake oil Salesmen who knows may be I am wrong )
xxxxxxxxxxxxxxxxxxxxxxxxx
21st November 2021:-
One friend made a sarcastic comment that may be Oxygen therapy can be given through the back side. He was not wrong at all. Good Outside the Box thinking on his lazy part.
Raju Jairam wrote :
There’s an effective way to get oxygenated via the rectum. It is done in the military hospitals, I think. It saves being intubated and is used when intubation is not an option due to injury. You might check it out.
xxxxxxxxxxxxxxxxx
Inspired by animals that breathe through their butts, scientists show that mammals can also harness the incredible breathing ability of our butts

Simon Spichak
Neuroscience
August 31, 2021 1 peer comment
Ed: Welcome to Butt Month. In the month of September, Massive will be publishing articles on the evolution, science, and technology surrounding the butt. If it touches the butt, we’ll be covering it. Why Butt Month? Why not. For previous butt stories, see the Butt Month page.
To survive in extreme low-oxygen conditions deep in the ocean, fish and other creatures have developed remarkable adaptations. For example, sea spiders, loaches, and catfish evolved the ability to breathe through their butts. And they might not be the only butt breathers out there.
A recent study in the journal Med now suggests that mammals, humans included, may be able to breathe through their rear ends as well. Mice, rats, and pigs could all stave off the devastating effects of oxygen deprivation if given an oxygen enema. But could this new method provide temporary oxygen while a patient awaits a ventilator?
Can Mammals Breathe Through Their Butt?
While we often consider the butt as the exit for waste in our body, it is also an entryway with lifesaving potential. After all, humans and plenty of other mammals can absorb medications rectally. That’s because there’s a lot of blood vessels in the area, allowing medicine easy entry.
But medicine is specially designed to maximize absorption in the body. Oxygen doesn’t have nearly as easy a path towards entry into the bloodstream through the rectum because of the mucus membrane mammals have on the intestines. There are also important anatomical differences between our intestines and those of fish that already harness this ability. Animals that can breathe through their butts, like loaches, had a much thinner epithelium in their guts and a lot less mucus. During the course of early development, a butt-breathing genetic pathway is turned on that helps dictate the structure of the intestine. When it’s all said and done, the posterior end of the intestine is equipped with all the structures necessary for respiration (and gas exchange).
Would this mucus prevent oxygenation in mice? In the first experiment, researchers used a model of oxygen deprivation in mice, preventing them from breathing through their lungs. The control group didn’t receive any intestinal ventilation, one group received oxygen through an anal catheter, and the final group had the mucus layer on their intestines “scrubbed” before receiving anal ventilation.
Remarkably, the mice supplied oxygen through their anus had elevated oxygen levels in their blood. The final group that also had their intestinal mucus scrubbed fared even better, surviving the longest in the low-oxygen conditions — five times as long as the control group. This experiment proved that there is potential for mammals to breathe through their butt, however, the mucus layer covering the intestinal epithelial cells makes it more difficult.
In a clinical setting, scrubbing the mucus off of a person’s intestines isn’t really feasible, and doesn’t sound like a pleasant experience. But using a method akin to an enema may work, by infusing safe, oxygenated liquid through the butt. This liquid, called perfluorodecalin, could safely store and deliver oxygen via an enema. Due to the properties of this liquid, it doesn’t need to scrub the mucus off of the intestines, meaning less discomfort and abrasion. Oxygen diffuses into the bloodstream while carbon dioxide diffuses out. Since it holds a lot of oxygen and carbon dioxide very easily, it is also delivered safely to the lungs, and is already in clinical use.
In their next experiment, mice were placed in chambers with only 10 percent oxygen. While this isn’t lethal, it is enough to induce the physiological effects of a lack of oxygen, hypoxia. The mice that received oxygen-loaded PFD rectally normalized their oxygenation back to normal levels.
In rats and pigs, the researchers repeated these experiments finding that two days of the protocol didn’t lead to any significant adverse effects. Importantly, the diffusion and distribution of many different drugs are tested in pigs due to similarities in physiology. While the authors couldn’t figure out how exactly the oxygen passes into the intestine, they showed enough efficacy to permit more studies trials in animals and in humans. According to the press release, the research team is working with Japan Agency for Medical Research and Development to conduct more experiments and potentially head to a human trial. This could increase the ventilation capacity of hospitals during future outbreaks of respiratory diseases.
Can Rectal Ventilation Mitigate a Ventilator Shortage?
During COVID-19, many hospitals find themselves short on ventilators. During the pandemic, many will require the use of a ventilator for an average of 15 days, while a few people will need significantly more time. Ventilators aren’t something that a person can use for one day and then get discharged. The first wave of people requiring ventilators will receive them immediately. However, someone whose lungs fail the next day may need to survive for two weeks without one.
In an interview with The Scientist, corresponding author Takanori Takebe, Assistant Professor, UC Department of Pediatrics and a Professor at the Institute of Research, Tokyo Medical and Dental University, Japan, explained how his father was hospitalized with acute respiratory distress syndrome due to a chronic lung condition. He saw first-hand how difficult and damaging mechanical ventilation can be on the body.
While these ventilators are the gold standard for treating acute respiratory distress syndrome, occurring through COVID-19 infection, it isn’t always available. In the intervening period, there is a need for more techniques and strategies to deliver oxygen and stave off hypoxia and death. If rectal ventilation can work in humans, it will provide a way for doctors to keep some of these people in a stable condition while they await a ventilator. Additionally, since there are no patents or complex mechanical components to rectal ventilation set up, it could be cost-effective to implement.
But humans aren’t pigs, or rats, or mice. Lots of incredible research and findings do not translate to humans. One problem remains unaddressed however how will patients or even animals receiving rectal ventilation poop? Can the enema be adjusted to facilitate bowel movements or could this tank the technology? Takebe will be working hard to test this method in more animal models and potentially a human clinical trial soon.
However, a company called Respirogen Inc. may beat him and his colleagues to it. Respirogen Inc. has registered a clinical trial to assess the safety of this method in healthy humans. Six healthy volunteers will experience induced hypoxia, by breathing in a mixture of gases with low oxygen content. In this study, these volunteers will then receive oxygen rectally to monitor whether this method can successfully increase oxygen levels and stave off symptoms of hypoxia. However, Respirogen Inc. will be using standard enemas and colonoscopy-cleansing procedures to reduce the chances someone will need to poop during the trial.
“In human use for treatment of hypoxia, cleansing of the colon will take place by standard enema or colonoscopy prep procedures, which are well understood and accepted,” Respirogen CEO Bob Scribner explained over email. “The use of an oxygen bolus delivery allows the procedure to be suspended and restarted as needed to accommodate a patient’s need to void.” Their technology uses an oxygen bolus, essentially a gas bubble, that is delivered into the butt, and could be stopped temporarily in case of a fecal emergency.
With at least two different groups working toward this goal, we may finally be able to say with some certainty, whether humans can effectively breathe through their butt. What sounds like a ridiculous question may end up saving people that aren’t immediately able to access a ventilator.
Peer Commentary
We ask other scientists from our Consortium to respond to articles with commentary from their expert perspective.

Namrata Iyer
Microbiology
Brown University
Link
Such a cool study. Thanks for highlighting it Simon and also putting it in the context of existing gold standard, the ventilator. You bring up a great point about how ventilators require a lot of specialized equipment, expertise and can cause lung injury themselves. An enema like procedure sounds a lot less painful and probably more accessible. I wonder if they tested for oxygen induced toxicity to the intestinal lining, and even the gut microbes. Though I guess that might be a relatively smaller cost if you are battling hypoxia. Excited to see how this technology develops!
 Simon Spichak responds
Simon Spichak respondsThanks for reading Namrata!
I think at that point, it really doesn’t matter what’s happening to your gut lining. I imagine it greatly disrupts the microbiome, which has microbes that usually don’t breathe in so much air. The animal study didn’t find any major signs of complications but they did not look at the microbiome. Either way doing this in humans is a whole other animal (pun intended) so it is unclear if it will work.
xxxxxxxxxxxxxxxxxxx
Peer-Reviewed Publication
TOKYO MEDICAL AND DENTAL UNIVERSITY
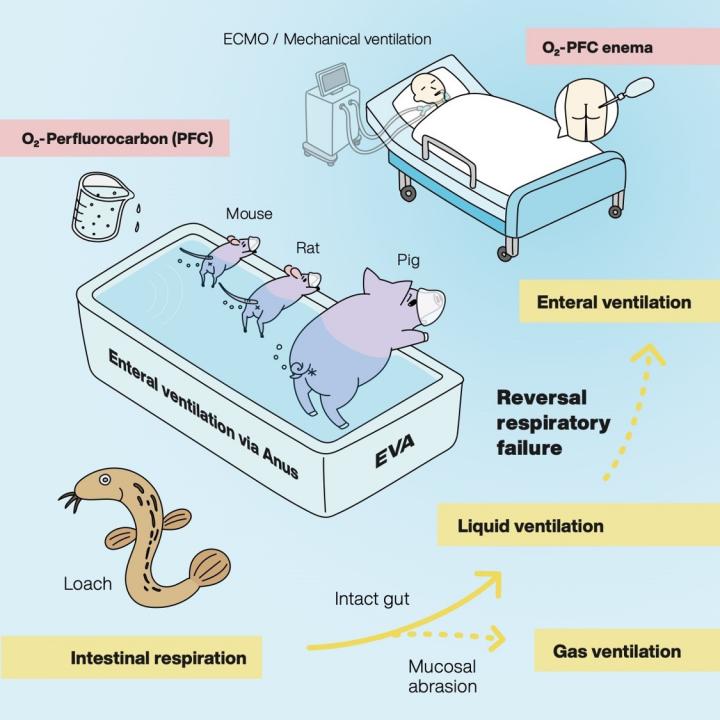
IMAGE: BASED ON THE FACT THAT LOACHES HAVE INTESTINAL RESPIRATION UNDER HYPOXIC CONDITIONS, THE EFFICACY OF THE EVA METHOD WAS EXAMINED IN MAMMALS SUCH AS MICE AND PIGS. THE EVA METHOD MAY BE EFFECTIVE FOR PATIENTS WITH RESPIRATORY FAILURE. view more
CREDIT: INSTITUTE OF RESEARCH,TMDU
Tokyo, Japan - Oxygen is crucial to many forms of life. Its delivery to the organs and tissues of the body through the process of respiration is vital for most biological processes. Now, researchers at Tokyo Medical and Dental University (TMDU) have shown that oxygen can be delivered through the wall of the intestine to compensate for the reduced availability of oxygen within the body that occurs in lung diseases that cause respiratory failure.
To breathe is to live; for higher animals, respiration involves absorbing oxygen and excreting carbon dioxide at gills or in the lungs. However, some animals have evolved alternative ventilatory mechanisms: loaches, catfish, sea cucumbers and orb-weaving spiders can absorb oxygen through their hindgut to survive in situations where the availability of oxygen is limited. Inspired by these unique adaptations, the team at TMDU devised strategies to allow gas exchange through the lining of the intestine, a process termed as enteral ventilation or EVA.
"The rectum has a mesh of fine blood vessels just beneath the surface of its lining, which means that drugs administered through the anus are readily absorbed into the bloodstream," first author Ryo Okabe explains. "This made us wonder whether oxygen could also be delivered into the bloodstream in the same way. We used experimental models of respiratory failure in mice, pigs and rats to try out two methods: delivering oxygen into the rectum in gas form, and infusing an oxygen-rich liquid via the same route."
The researchers prepared the lining of the rectum by rubbing it to cause inflammation and increase blood flow; these changes were confirmed by increased genetic markers and improved the effectiveness of the oxygen delivery. However, because such a preparation requirement would be unacceptable for human patients, the researchers also tried using oxygenated perfluorodecalin (PFD), a liquid that can be safely used in the human body and is already in selective clinical use, and that can carry large amounts of oxygen and carbon dioxide.
The team demonstrated that delivery of oxygen both as a gas and in liquid form was beneficial: oxygenation levels increased and behavior normalized, while survival was prolonged. The team also confirmed the improvement in oxygenation at the cellular level by immunochemical staining. Furthermore, they found that the minimal amount of PFD that was absorbed along with the oxygen caused no harm, and gut bacteria were not disrupted, indicating the safety of these methods in the animal models.
"Patients in respiratory distress can have their oxygen supply supported by this method to reduce the negative effects of oxygen deprivation while the underlying condition is being treated," foresees Takanori Takebe, corresponding author. "Enteral ventilation showed great promise in our asphyxia-like experimental model. The next steps will be to test safety of the EVA approach with more profound mechanistic understanding by which it works; and to establish effectiveness in humans in a clinical setting."
Conventional therapeutic respiratory support comprises complex technological protocols such as ventilators and artificial lungs. The current SARS-CoV-2 pandemic has highlighted the high need for development of less invasive alternatives such as EVA for short-term support of respiratory function. These new findings from the researchers at TMDU may pave the way for new ventilation strategies in the future.
###
The article, "Mammalian Enteral Ventilation Ameliorates Respiratory Failure" was published in Med at DOI:10.1016/j.medj.2021.04.004
TOKYO MEDICAL AND DENTAL UNIVERSITY
IMAGE: BASED ON THE FACT THAT LOACHES HAVE INTESTINAL RESPIRATION UNDER HYPOXIC CONDITIONS, THE EFFICACY OF THE EVA METHOD WAS EXAMINED IN MAMMALS SUCH AS MICE AND PIGS. THE EVA METHOD MAY BE EFFECTIVE FOR PATIENTS WITH RESPIRATORY FAILURE. view more
CREDIT: INSTITUTE OF RESEARCH,TMDU
Tokyo, Japan - Oxygen is crucial to many forms of life. Its delivery to the organs and tissues of the body through the process of respiration is vital for most biological processes. Now, researchers at Tokyo Medical and Dental University (TMDU) have shown that oxygen can be delivered through the wall of the intestine to compensate for the reduced availability of oxygen within the body that occurs in lung diseases that cause respiratory failure.
To breathe is to live; for higher animals, respiration involves absorbing oxygen and excreting carbon dioxide at gills or in the lungs. However, some animals have evolved alternative ventilatory mechanisms: loaches, catfish, sea cucumbers and orb-weaving spiders can absorb oxygen through their hindgut to survive in situations where the availability of oxygen is limited. Inspired by these unique adaptations, the team at TMDU devised strategies to allow gas exchange through the lining of the intestine, a process termed as enteral ventilation or EVA.
"The rectum has a mesh of fine blood vessels just beneath the surface of its lining, which means that drugs administered through the anus are readily absorbed into the bloodstream," first author Ryo Okabe explains. "This made us wonder whether oxygen could also be delivered into the bloodstream in the same way. We used experimental models of respiratory failure in mice, pigs and rats to try out two methods: delivering oxygen into the rectum in gas form, and infusing an oxygen-rich liquid via the same route."
The researchers prepared the lining of the rectum by rubbing it to cause inflammation and increase blood flow; these changes were confirmed by increased genetic markers and improved the effectiveness of the oxygen delivery. However, because such a preparation requirement would be unacceptable for human patients, the researchers also tried using oxygenated perfluorodecalin (PFD), a liquid that can be safely used in the human body and is already in selective clinical use, and that can carry large amounts of oxygen and carbon dioxide.
The team demonstrated that delivery of oxygen both as a gas and in liquid form was beneficial: oxygenation levels increased and behavior normalized, while survival was prolonged. The team also confirmed the improvement in oxygenation at the cellular level by immunochemical staining. Furthermore, they found that the minimal amount of PFD that was absorbed along with the oxygen caused no harm, and gut bacteria were not disrupted, indicating the safety of these methods in the animal models.
"Patients in respiratory distress can have their oxygen supply supported by this method to reduce the negative effects of oxygen deprivation while the underlying condition is being treated," foresees Takanori Takebe, corresponding author. "Enteral ventilation showed great promise in our asphyxia-like experimental model. The next steps will be to test safety of the EVA approach with more profound mechanistic understanding by which it works; and to establish effectiveness in humans in a clinical setting."
Conventional therapeutic respiratory support comprises complex technological protocols such as ventilators and artificial lungs. The current SARS-CoV-2 pandemic has highlighted the high need for development of less invasive alternatives such as EVA for short-term support of respiratory function. These new findings from the researchers at TMDU may pave the way for new ventilation strategies in the future.
###
The article, "Mammalian Enteral Ventilation Ameliorates Respiratory Failure" was published in Med at DOI:10.1016/j.medj.2021.04.004
xxxxxxxxxxxxxxxxxxxxxxxxxxx
JUN. 7, 2021NEWS
Lung Diseases
The Problem: Patients suffering from lung failure are often put on ventilators, but as we have seen during the COVID-19 pandemic, these tools aren’t always readily available and can run out.
The Study: ‘Breathing through the rectum’ via a suppository containing oxygen seems to be a surprisingly effective strategy for treating oxygen deprivation, finds a new study in mice and pigs published in Med by NYSCF – Robertson Stem Cell Investigator Takanori Takebe, MD of Cincinnati Children’s Hospital and Tokyo Medical and Dental University.
Why it Matters: This study demonstrates the great potential of this new oxygen delivery system as a simple and scalable way to treat patients suffering from low oxygen.
Dr. Takebe was inspired to explore new solutions for low oxygen after watching his father’s battle with lung disease. He observed during the height of the pandemic that ventilator supply is limited, and started thinking about how we may be able to deliver oxygen by leveraging organs other than the lungs.
“We clearly need different strategies to help out patients with severe lung failure,” he told The New York Times.
Dr. Takebe turned his attention to the animal kingdom – specifically, fish. He learned that some fish absorb oxygen through their gills, but can also bob their heads above the water to breathe in air, which they absorb through their intestines.
Could mammalian intestines also absorb oxygen? Dr. Takebe first tested this theory by delivering oxygen gas to anesthetized, oxygen-deprived pigs and mice via their rectums. The method worked, but getting it to the required efficacy meant thinning out the intestinal walls – not very appealing for human patients.
The team then wondered whether a liquid would solve the problem. They used a perfluorochemical – a liquid that can absorb gases – to deliver oxygen to the pigs and mice through their rectums, and saw marked improvements in the animals’ oxygen levels. Mice regained their ability to walk, and the pigs’ pale skin returned to its signature pink.
“They are completely recovering from the very, very severe hypoxia,” said Dr. Takebe. “That was really astonishing to me.”
The method, while unconventional, makes sense given what we know about the body. The colon’s thin walls are particularly adept at delivering substances to the body (think: suppositories), and doctors have long known that the GI tract can absorb gases.
Next, Dr. Takebe hopes to adapt this method for human patients in need.
“I am really keen on pursuing the clinical translation potentials as fast as possible,” he said.
His new startup, EVA (an acronym for ‘enteral ventilation via anus’) is aiming to move the technique into clinical trials as soon as next year.
Caleb Kelly, MD, PhD, a gastroenterology fellow at Yale University who reviewed Dr. Takebe’s study, urges people to set aside their initial reactions to the method’s, well, ‘weirdness’, and focus on the results.
“It’s kind of a startling idea, to use that part of human anatomy for gas exchange,” he said. “But it really should be the data, rather than our visceral reactions to the concept, that guide us.”
Journal Article:
Mammalian enteral ventilation ameliorates respiratory failure
Ryo Okabe, Toyofumi F. Chen-Yoshikawa, Yosuke Yoneyama, Eiji Kobayashi, Hiroshi Date, Takanori Takebe. Med. 2021. DOI: https://doi.org/10.1016/j.medj.2021.04.004
xxxxxxxxxxxxxxxxxxxxxxxx
Lung Diseases
The Problem: Patients suffering from lung failure are often put on ventilators, but as we have seen during the COVID-19 pandemic, these tools aren’t always readily available and can run out.
The Study: ‘Breathing through the rectum’ via a suppository containing oxygen seems to be a surprisingly effective strategy for treating oxygen deprivation, finds a new study in mice and pigs published in Med by NYSCF – Robertson Stem Cell Investigator Takanori Takebe, MD of Cincinnati Children’s Hospital and Tokyo Medical and Dental University.
Why it Matters: This study demonstrates the great potential of this new oxygen delivery system as a simple and scalable way to treat patients suffering from low oxygen.
Dr. Takebe was inspired to explore new solutions for low oxygen after watching his father’s battle with lung disease. He observed during the height of the pandemic that ventilator supply is limited, and started thinking about how we may be able to deliver oxygen by leveraging organs other than the lungs.
“We clearly need different strategies to help out patients with severe lung failure,” he told The New York Times.
Dr. Takebe turned his attention to the animal kingdom – specifically, fish. He learned that some fish absorb oxygen through their gills, but can also bob their heads above the water to breathe in air, which they absorb through their intestines.
Could mammalian intestines also absorb oxygen? Dr. Takebe first tested this theory by delivering oxygen gas to anesthetized, oxygen-deprived pigs and mice via their rectums. The method worked, but getting it to the required efficacy meant thinning out the intestinal walls – not very appealing for human patients.
The team then wondered whether a liquid would solve the problem. They used a perfluorochemical – a liquid that can absorb gases – to deliver oxygen to the pigs and mice through their rectums, and saw marked improvements in the animals’ oxygen levels. Mice regained their ability to walk, and the pigs’ pale skin returned to its signature pink.
“They are completely recovering from the very, very severe hypoxia,” said Dr. Takebe. “That was really astonishing to me.”
The method, while unconventional, makes sense given what we know about the body. The colon’s thin walls are particularly adept at delivering substances to the body (think: suppositories), and doctors have long known that the GI tract can absorb gases.
Next, Dr. Takebe hopes to adapt this method for human patients in need.
“I am really keen on pursuing the clinical translation potentials as fast as possible,” he said.
His new startup, EVA (an acronym for ‘enteral ventilation via anus’) is aiming to move the technique into clinical trials as soon as next year.
Caleb Kelly, MD, PhD, a gastroenterology fellow at Yale University who reviewed Dr. Takebe’s study, urges people to set aside their initial reactions to the method’s, well, ‘weirdness’, and focus on the results.
“It’s kind of a startling idea, to use that part of human anatomy for gas exchange,” he said. “But it really should be the data, rather than our visceral reactions to the concept, that guide us.”
Journal Article:
Mammalian enteral ventilation ameliorates respiratory failure
Ryo Okabe, Toyofumi F. Chen-Yoshikawa, Yosuke Yoneyama, Eiji Kobayashi, Hiroshi Date, Takanori Takebe. Med. 2021. DOI: https://doi.org/10.1016/j.medj.2021.04.004
xxxxxxxxxxxxxxxxxxxxxxxx
COVID-19: Researchers find new routes for oxygen
Ventilators are in high demand because of COVID-19. Supply is tight. As an alternative, could we get oxygen through our backsides? It's not as odd as you might think.

The COVID-19 pandemic has pushed intensive care units to the limit
Japanese researchers say mammals can breathe through their intestines.
The researchers put pigs and rodents in life-threatening situations by reducing oxygen flow, and then prevented respiratory failure by delivering oxygen via the animals' rectums.
Their findings, published in the journal Med, could pave the way for new therapies to balance oxygen levels in humans when their lungs fail, and mechanical ventilation is limited or unavailable — as is often the case for COVID-19 patients who need intensive care.
"Artificial respiratory support plays a vital role in the clinical management of respiratory failure due to severe illnesses, such as pneumonia or acute respiratory distress syndrome," write the researchers, including lead author Takanori Takebe, of the Tokyo Medical and Dental University.
"Although the side effects and safety need to be thoroughly evaluated in humans, our approach may offer a new [way] to support critically ill patients with respiratory failure," Takebe said in a Cell Press article.
Takebe said the inspiration for the research came from some aquatic organisms that are known to breathe from the gut.

Researchers in Kenya and worldwide are seeking new ideas for ventilation systems
So the researchers wanted to see whether the same was true in mice, rats and pigs — common animal subjects new ideas are tested on humans.
"Also, we know that [parts] of the rectum are suitable for drug or nutrient absorption," Takebe said.
The rectum can serve as a route to administer drugs or fluids, which are then absorbed by blood vessels and flow into the body's circulatory system.
Oxygenation like an enema
The researchers injected oxygen through the rectums of anesthetized mice in an oxygen-deprived environment, using an enemalike procedure.
An enema involves inserting a liquid into the rectum or colon by way of the anus. Simple enemas from a pharmacy may consist of a bottle and nozzle with a liquid solution.
In their study, the researchers say that mice died after 11 minutes of extremely low-oxygen conditions.
But they say that when they used their method of providing oxygen through the rectum, 75% of mice survived 50 minutes of deadly low-oxygen conditions.
Limited application
The procedure is "limited to 20-60 minutes and is not a permanent rescue," the researchers said.
They said they also had to scrape the intestinal lining for the method to work.
That makes it unlikely to be clinically feasible, especially in severely ill patients, they said. And other experts in the field agree.
"The intestine was scraped to thin it so that oxygen could be absorbed by thin membranes, and that showed the improved oxygenation," Dr. Akshay Budhraja, a pulmonary consultant at the Aakash Healthcare Super Speciality Hospital in New Delhi, told DW.
"But this idea seems impractical on humans, considering the complex human anatomy and the procedure of thinning the intestine or any other visceral layer in a sick patient," Budhraja said.
Budharaja was not involved in the Japanese study. But India is battling an intensive wave of COVID-19 infections and has a shortage of traditional ventilation machines as a result. So, any new research would be welcome. And not only there.
The pandemic has overwhelmed the need for ventilators worldwide.
Ventilators are machines that pump air into the lungs to keep sick or injured patients who cannot breathe sufficiently themselves alive.
The researchers injected oxygen through the rectums of anesthetized mice in an oxygen-deprived environment, using an enemalike procedure.
An enema involves inserting a liquid into the rectum or colon by way of the anus. Simple enemas from a pharmacy may consist of a bottle and nozzle with a liquid solution.
In their study, the researchers say that mice died after 11 minutes of extremely low-oxygen conditions.
But they say that when they used their method of providing oxygen through the rectum, 75% of mice survived 50 minutes of deadly low-oxygen conditions.
Limited application
The procedure is "limited to 20-60 minutes and is not a permanent rescue," the researchers said.
They said they also had to scrape the intestinal lining for the method to work.
That makes it unlikely to be clinically feasible, especially in severely ill patients, they said. And other experts in the field agree.
"The intestine was scraped to thin it so that oxygen could be absorbed by thin membranes, and that showed the improved oxygenation," Dr. Akshay Budhraja, a pulmonary consultant at the Aakash Healthcare Super Speciality Hospital in New Delhi, told DW.
"But this idea seems impractical on humans, considering the complex human anatomy and the procedure of thinning the intestine or any other visceral layer in a sick patient," Budhraja said.
Budharaja was not involved in the Japanese study. But India is battling an intensive wave of COVID-19 infections and has a shortage of traditional ventilation machines as a result. So, any new research would be welcome. And not only there.
The pandemic has overwhelmed the need for ventilators worldwide.
Ventilators are machines that pump air into the lungs to keep sick or injured patients who cannot breathe sufficiently themselves alive.
Previous trials in Spain
The idea of "anal oxygenation" has been tested before. Researchers tried it on human COVID-19 patients in a small study in Spain in 2020.
Their study, published in the journal SN Comprehensive Clinical Medicine, evaluated the effectiveness of introducing ozone through the rectum in four COVID-19 patients with severe pneumonia.
They found that rectal ozone improved levels of oxygen in the blood and decreased inflammation in patients with severe COVID-19 pneumonia. Ozone is a gas made up of three oxygen atoms.
The authors concluded that rectal ozone was an effective, safe, cheap and simple alternative for the management of severe pneumonia in COVID-19 patients.
Other health benefits
The Japanese study, meanwhile, found that administering liquid oxygen through the intestines also provided therapeutic benefits to rodents and pigs exposed to nonlethal low-oxygen conditions.
Mice receiving the therapy could walk farther in an oxygen-deprived chamber. More oxygen reached the heart, compared to those that did not receive oxygen through the rectum.
The researchers found similar results in pigs, who share more physiology with humans than mice.
Promise in humans
The Japanese scientists said that if the new method of injecting oxygen through the anus were scaled for human application, it could be used to treat patients with severe respiratory failure as seen in COVID-19 patients.
Budhraja said there was still a long way to go for the method to be effectively used in humans.
Intestines have a limited capability to exchange gas, Budhraja said, which means that they may not be able to maintain an optimum oxygen level in life-threatening situations and prevent damage to vital organs.
Takebe said more work would need to be done to "cautiously evaluate" the safety of the process in humans. The team plans to expand its preclinical studies and apply for permission to carry out the clinical trials within the next two years.

xxxxxxxxxxxxxxxxxxxxxxxx
xxxxxxxxxxxxxxxxxxxxxxxx
Summary:
1 - Yes it is possible to Oxygenate the blood via the rectum
2 - "Oxygen doesn’t have nearly as easy a path towards entry into the bloodstream through the rectum because of the mucus membrane mammals have on the intestines. "
3 - we may eat or swallow pills that could produce oxygen in the stomach but the mucous membrane lining the small intestines will prevent absorption
xxxxxxxxxxxxxxxxxx
HOW ABOUT DEVELOPING SUPPOSITORIES THAT RELEASE OXYGEN SLOWLY IN THE RECTUM
30th November 2021
Scientist from the City of Joy Invents ‘Pocket Ventilator’
June 11, 2021

News Desk: “Pocket ventilator” that might turn out to be a savior in this pandemic situation has been invented by a scientist in Kolkata. Dr Ramendra Lal Mukherjee, is an engineer by profession and loves experimenting and innovating new gadgets. This time he has developed a portable, battery-operated pocket-sized ventilator which can give instant assistance to patients with breathing difficulty. Non-invasive and cheap, it can be an effective alternative for the heavy CPAP (continuous positive airway pressure) device used in hospitals.
Mukherjee shares that recently he contracted Covid-19 infection and his Oxygen saturation went down drastically.
“There was a point when my SpO2 level went down to 88. At that time my family wanted me to get admitted to a hospital. Though I came out of the crisis, I was struck by the idea of a portable device to help patients breathe easy,” he tells.
Post his recovery he began working on the plan, got essential parts, and finally designed the pocket ventilator. His innovation was ready in just 20 days.
This device, he explained, consists of two parts – a power unit and a ventilator unit attached to the mouthpiece. Once the ventilator is turned on it extracts air from outside and pass it through an ultra-violet (UV) chamber so that it can be free of viruses and germs. It then flows into the mask attached to the device developing an impetus which boosts the airflow into the respiratory system of the patient. On the other hand, the exhaled carbon dioxide, is piped through another UV chamber before it gets discharged out.
“This ensures that even if a person is infected with Covid, the UV filter kills the virus before the air is discharged out of the device after it is exhaled. This will ensure reduced transmission of the virus and doctors will feel more protected,” Mukherjee clarifies.
xxxxxxxxxxxxxxxxxx

News Desk: “Pocket ventilator” that might turn out to be a savior in this pandemic situation has been invented by a scientist in Kolkata. Dr Ramendra Lal Mukherjee, is an engineer by profession and loves experimenting and innovating new gadgets. This time he has developed a portable, battery-operated pocket-sized ventilator which can give instant assistance to patients with breathing difficulty. Non-invasive and cheap, it can be an effective alternative for the heavy CPAP (continuous positive airway pressure) device used in hospitals.
Mukherjee shares that recently he contracted Covid-19 infection and his Oxygen saturation went down drastically.
“There was a point when my SpO2 level went down to 88. At that time my family wanted me to get admitted to a hospital. Though I came out of the crisis, I was struck by the idea of a portable device to help patients breathe easy,” he tells.
Post his recovery he began working on the plan, got essential parts, and finally designed the pocket ventilator. His innovation was ready in just 20 days.
This device, he explained, consists of two parts – a power unit and a ventilator unit attached to the mouthpiece. Once the ventilator is turned on it extracts air from outside and pass it through an ultra-violet (UV) chamber so that it can be free of viruses and germs. It then flows into the mask attached to the device developing an impetus which boosts the airflow into the respiratory system of the patient. On the other hand, the exhaled carbon dioxide, is piped through another UV chamber before it gets discharged out.
“This ensures that even if a person is infected with Covid, the UV filter kills the virus before the air is discharged out of the device after it is exhaled. This will ensure reduced transmission of the virus and doctors will feel more protected,” Mukherjee clarifies.
xxxxxxxxxxxxxxxx
Thursday 9th Dec 2021
My Discussion with Prof Mutharasan my buddy & mentor
Me: Muthu, the fine capillaries in the lungs absorb oxygen, now we know that fine capilllaries in the rectum and large intestine can absorb oxygen and raise the oxygen saturation.
Why cant we trick and make blood vessels in our skin absorb oxygen ?
Like the feet immersed in an oxygen bath.
We do Dialysis where we take the entire blood out of the body, filter it like the kidney does and put it back into the body.
Surely there has to be a way to oxygenate the blood in a dialysis machine. There has to be a way.
Please ask around and some one might have an out of the box answer.
Muthu Wrote: Heart-Lung Machine adds oxygen to blood. Transfer of oxygen via skin might occur (will check) but it is very small compared to our body's oxygen need. Key parameter in this is solubility of oxygen, which is very small (about 7 parts/million, or 7 mg Oxygen per liter of blood) and thus large surface area is needed. Our skin's area is not large compared to the interfacial area of the lungs (will give numbers after checking with my physiology book).
Just checked- skin does breathe in oxygen, but at a very low rate, approx. one milliliter per square meter of skin per minute
Me: That is good news Muthu, all we need to do is find some accelerant muthu and you will get a Nobel Prize. Trust me
Muthu: I like your problem solving attitude, keep chugging, mate!
Me: Muthu, Now I am going to pick on your Brains. assuming you have two independent lobes. I don't want to hear that it cannot be done as every second fool will say that even without thinking. Let me know only when You believe it is possible Ok 👇👇👇👇
How about developing suppositories that release oxygen slowly into the rectum to be absorbed by the blood vessels lining the rectum ?
Me: I cant stop Thinking of Finding an easier way to Oxygenate the blood relieving the already struggling lung and heart of overload like using ECMO. Every one laughed and Then I was able to prove that blood oxygen saturation levels can be raised through Oxygen in the Rectum as done in Japan and Africa. If we can take the blood out of the body perform dialysis and filter the blood doing the work of the Kidneys and putting the Blood Back, why cannot we also oxygenate the blood at the same time. Even this to me meaning Dialysis is not a simple procedure. My new line of thinking 100 % of the Human skeletal system is Covered by SKIN. The skin as we know Breathes in colloquial terms. Meaning it can sweat and push out Toxins. How about an Oversized High pressure suit like used by scuba divers seal it off at the neck to avoid leaks and then pressurise the suit with with JUST Pure OXYGEN plus some accelerant to make the fine capillaries in the skin absorb the oxygen straight into the blood and the lungs as always can expel the Co2. I know you said the skin absorbs a small amount of Oxygen from then atmosphere, But the atmospheric air is not 100% Oxygen. How do we make the or Retrain the skin skin Absorb Oxygen. The Human brain is wired in such a way that when there is any kind of shortage of water or oxygen or sugar etc to make effective changes to adapt and compensate. When sugar levels are too low the Liver pumps glycogen into the blood stream to keep brain cells alive.
Surely the Brain will sense hey there is so much oxygen around the body let us make hay when the sun shines. Can I ask you to have a general discussion on this with your son and Dil who are both specialist Cardiologist and endocrinologist
xxxxxxxxxxxxxxxxxx






No comments:
Post a Comment